David Lareau is CEO of Medicomp Systems of Chantilly, VA.
Wallis Simpson, the divorced American socialite who was the mistress and later wife of Prince Edward of Wales, famously once said, “You can never be too rich or too thin.” I assume that Edward concurred because he abdicated the British throne to become her husband.

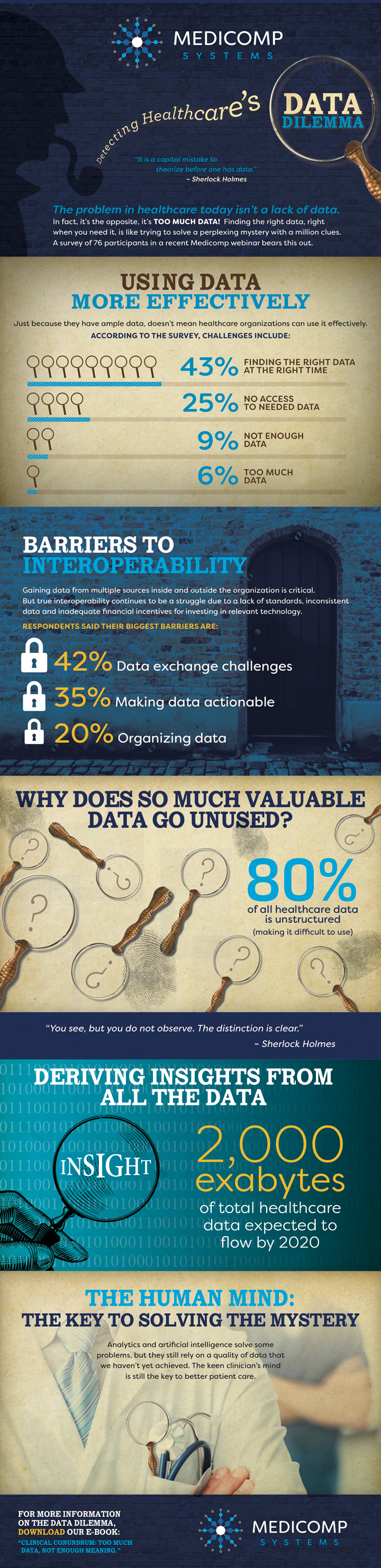
I don’t worry too much about being too rich or thin. My worries tend to be about more mundane topics – like fixing the dilemma of too much data. Before the widespread adoption of EHRs, most providers figured you could never have too much data. But today we have an explosion of clinical data – and are predicted to have 2,000 exabytes worth by the year 2020. With so much data, providers are now struggling to find the data they need, when they need it, to derive meaningful insights.
In fact, in a recent webinar, 43 percent of our participants claimed that their top data-related challenge was finding the right data at the right time. Of the 76 healthcare IT professionals and physicians participating in the survey, 25 percent said they didn’t have access to the data they needed; 9 percent reported not having enough data; and 6 percent complained of having too much data.
Data obviously plays an important role in decision-making. Even if you have ample data, it’s difficult to make sense of things if you can’t access the data you need when and where you need it. Consider what happens when a physician sees a patient and lacks ready access to their medical history, problem lists, medications, and test results. Without access to the results of a critical test, the provider may re-order the identical test, possibly wasting healthcare resources and creating confusion about the accuracy of the patient’s records.
Adding to providers’ data dilemmas is a lack of true interoperability between systems. We asked our webinar participants about their biggest barriers to achieving interoperability and 42 percent pointed to the challenge of data exchange. An additional 35 percent expressed difficulty applying data and making it actionable, while 20 percent reported difficulties organizing the data they received.
Even though new exchange standards, such as FHIR, are making it easier to send data between providers, the incoming data is usually highly disorganized and not stored in an easily searchable format that adds value for clinical decision-making. In fact, the flood of incoming, unorganized data, makes it easy for providers to overlook critical information – and put themselves at increased medical liability risk, should the patient end up with health complications.
Making the “too much data” worse is the fact that an estimated 80 percent of all health data is stored in as free-text notes, scans, or other unstructured formats that are difficult to organize and search, and often contain numerous duplicates. New technologies such as natural language processing (NLP) and artificial intelligence (AI) may eventually help providers to convert free-text data to actionable formats, but today these tools are not sufficiently mature to support clinical decision-making.
To fix the “too much data” problem, providers need tools such as Quippe Clinical Solutions to intelligently identify, interpret, and link medical concepts and map them to standard nomenclature, such as ICD-10, SNOMED, RxNorm, and LOINC. Data can be made usable for use at the point of care, allowing clinicians to easily find the information they need during patient encounters and within their normal workflows. The structured data is also properly formatted for input into AI systems that use advanced algorithms to deliver additional clinical insights.
Quippe Clinical Solutions help providers solve their “too much data” problems. But if you are feeling too rich and thin, I’ll have to defer to Wallis Simpson.
To learn more about the data tsunami, check out our new infographic.