Every few years, the healthcare industry seems to lose its collective mind over the latest new thing that will solve all our problems and usher in the (dreaded) “new paradigm.” This combination of magical thinking and marketing hype sporadically erupts and then dissipates as reality sets in, and we realize that there is no single answer to the challenges we face.
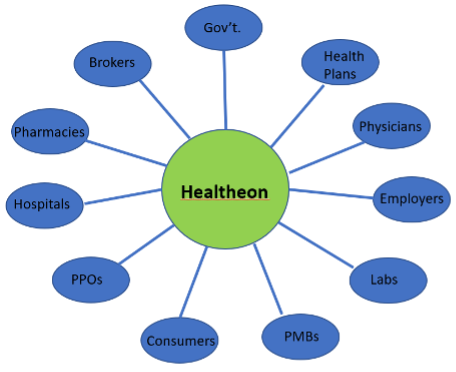
This boom-and-bust cycle has been going on for years. One of the best examples is described in Michael Lewis’ 1999 book “The New, New Thing,” which details the founding of Healtheon, which was going to connect every healthcare enterprise––enabling seamless exchange of information. The governing concept was presented in the book, and in presentations to investors, using what Lewis called “the chart of many bubbles”:
At about the same time as “The New, New Thing” was published, DrKoop.com raised $84M in an IPO, and the hype cycle became a near-annual event, often culminating in a blizzard of press releases leading up to the HIMSS conference announcing multiple next new things that would each change everything.
Now, think back … can you recall the seismic buzz surrounding the following developments?
- National terminology standards and free access to SNOMED to promote “semantic interoperability”
- Free EHRs
- Sam’s Club selling EHRs
- Big Data
- Microsoft Health Vault and Google Health
- Meaningful use and the ‘post-EHR’ world
- Personalized medicine
- Social determinants of health
- Natural language processing (curiously, always three to five years away)
- Patient engagement
Now, fast-forward to one of the latest new things––one that has garnered considerable buzz for the last few years: The notion that, even though clinical usability remains a major issue for healthcare IT, there’s no need to worry about it because the solution is at hand. That solution: Ambient AI capturing sound and video in the exam room, using NLP to turn it into data, and applying machine learning to make it so that clinicians don’t need to interact with the system.
Meanwhile, while we wait for this magical solution, scribes can interact with the system so that clinicians don’t need to, and post-encounter processing will do the rest––including quality measures, documentation review and validation, and coding.
Don’t get me wrong. Most of the technologies that have been generating the buzz do have an important role in addressing clinical usability, interoperability, the use of data analytics to improve population health, and using voice, artificial intelligence, and machine learning to ease the burden on clinicians. However, all these things must work together to provide clinicians with the information they need, at the point of care, to improve patient care and achieve better outcomes.
Ultimately, the real magical thinking is that any one thing is going to be the fabled magic bullet.
There is a better way. Providing tools to enable the most powerful computer at the point of care––the clinician’s brain––to find, act upon, and record clean, relevant clinical data will lead to improvements in usability, interoperability and, most importantly, better clinical outcomes.
On paper, it sounds simple. But delivering usable content to healthcare IT’s ‘last mile’ is much more complicated and will require widespread implementation of the standards, and the ability to receive, consolidate, and make sense of all that information.
In my next series of “A Different Point of View” posts, we’ll drill down into what it will take to tackle the ‘last mile’ challenge, and how the 21st Century Cures act and TEFCA will require new tools that empower clinicians at the point of care to deliver better patient outcomes.
###
